Joseph R. Anticaglia MD
Medical Advisory Board
Former President Jimmy Carter was hospitalized and underwent surgery at Emory University Hospital in November, 2019 to relieve pressure in his brain. The 95 year old and 39th president of the U. S. suffered a head injury after falling which his doctors described as a subdural hematoma (SDH).
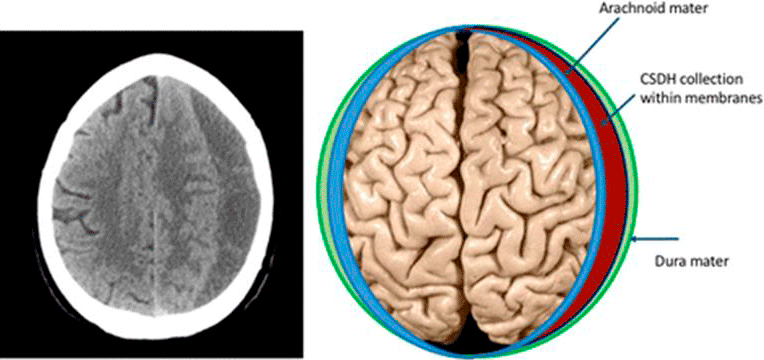
Subdural hematoma is a collection of blood between the skull and the brain. The brain is covered by the meninges, a three layered membrane whose outer layer is the dura mater, the middle layer is the arachnoid mater and the inner layer is the pia mater that covers the brain.
The skull is an unyielding, tight space. If there’s bleeding within this space, pressure builds up, distorting the brain causing life threatening symptoms. In patients with a subdural hematoma, blood accumulates beneath the dura mater.
The elderly are more prone to falls and balance problems and President Carter is no exception. In older patients, the brain shrinks and the meningeal blood vessels stretch and are more susceptible to burst.
In May of 2019, Mr. Carter fell and fractured his hip; on October 6, 2019, he fell, hit his head requiring 14 stiches and about two weeks later (Oct. 21), he fell and fractured his pelvis. Most recently, on November 3, 2019, he fell and suffered a subdural hematoma. Nine days later, he underwent a procedure to remove the SDH and relieve the intracranial pressure.
Subdural Hematoma Risk Factors
- Very young or very old
- Repeated head injuries (e. g. from falls)
- Medications that thin the blood (aspirin, warfarin)
- People diagnosed with a seizure disorder
- Alcohol abuse
- Medical conditions that causes your blood to clot poorly (hemophilia, deficiency of blood clotting factors)
Acute vs. Chronic Subdural Hematoma
‘Acute’ SDH is the bleeding that occurs after a serious blow to the head, for instance, after a car accident. A short time after the blow to the head, blood accumulates beneath the dura mater and intracranial pressure rises. The patient may be unconscious and emergency surgery is often needed to relieve the pressure within the brain and save the person’s life.
Chronic SDH
‘Chronic’ SDH is intracranial bleeding that occurs slowly, often in the elderly, after a relatively minor blow to the head. It may take weeks or months before the symptoms of SDH to appear.
Stephanie is a 76 year old lady who takes aspirin daily and is treated for hypertension and high cholesterol. In the middle of the night she slipped, fell and bumped her dead on the night table. She did not lose consciousness and examination of the head showed no evidence of swelling, bruising nor a cut or tear of the skin in the scalp.
But she had an excruciating headache over the forehead that persisted for 36 hours. Within the following 24 hours she was examined by her internist, had a CT scan of the brain done (computed tomography) and was referred to a neurosurgeon who reviewed the images of the CT who said:
“Good news! We don’t have to operate,” said the neurosurgeon. “You do have bleeding within the brain but there’s no localized accumulation of blood causing pressure on the brain. Stop taking aspirin and we’ll repeat the CT in four to six weeks. I anticipate that your body will absorb the blood over the next several weeks. It might even take a few months. You don’t need medication except for pain that should gradually lesson. If you have other symptoms beside the headache, call me immediately.”
Symptoms
Symptoms depend on the severity of the head injury, the size and location of the hematoma, that is, where it presses on the brain. One or more of the following symptoms may be present.
- Unconsciousness
- Severe headache
- Confusion, memory loss
- Trouble speaking
- Difficulty walking
- Gastrointestinal problems — loss of appetite, nausea, vomiting
- Drowsiness; (it could be side effect of taking medications for headache or other pain)
- Seizure
- Weakness or numbness of arms, legs, face
- Problems with vision
Diagnosis
Patients require a complete neurologic examination. The best diagnostic tool is to obtain a CT scan of the brain and reviewing the findings with the patient. It will help determine whether or not surgery is needed to treat the person’s head injury.
Treatment
The goal of treatment is to alleviate symptoms, prevent complications and permanent brain damage. In Stephanie’s case, no treatment was necessary except pain medication and reassurance that most of the time her body will reabsorb the blood in the subdural space.
In other instances, surgery is indicated, and not infrequently, on an emergency basis to relieve the buildup of pressure in the brain. This may include making small holes in the skull, or at other times, larger openings to remove the accumulated blood.
Complications
SDH can cause a wide range of short or long-term complications. It can affect thinking and memory, trouble speaking-communicating and personality changes. It may lead to chronic headache, seizures and permanent brain damage. Depending on the severity and location of the head injury and blood collection, the mortality rate has been reported to be greater than 50% in such cases.
The young and the elderly are particularly susceptible to acute and chronic subdural hematomas. The prognosis depends on the size and location of the hematoma and how soon treatment is started. SDH demands prompt evaluation and treatment to control symptoms, prevent complications and to save lives.
References
- Ellie Edlmann et al; Pathophysiology of chronic subdural haematoma; inflammation, angiogenesis and implications for pharRmacotherapy; Journal of Neuroinflammation; May 30, 2017
- Tandon PN; Acute subdural haematoma. a reappraisal; Neurology India, 2001
- Acute Subdural Hematomas; UCLA Neurosurgery, Los Angeles, CA
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.

