Joseph R. Anticaglia MD
Medical Advisory Board
Trauma is the most common cause of death in young people. And almost half of these trauma-related deaths are caused by head injury. It’s estimated that over 50,000 deaths a year in the United States is attributed to head injury.
In 2014, according to the CDC, there were approximately “2.87 million brain injury-related emergency department visits and hospitalizations in the US” due to head trauma. Children accounted for 870,000 of these medical events.
Traumatic brain injury (TBI) is any external injury to your scalp, skull or brain. It can range from a mild scalp wound, to skull fractures, to life threatening brain injuries.
It’s called a closed brain injury when there’s no skull fracture which can happen after a sport’s injury or car accident. In this instance, the rapid backward and forward movement tears and bruises the brain tissue, nerves and blood vessels (coup-contrecoup injury)
It’s called a open/penetrating brain injury when there is a fracture-break in the skull and an object penetrates the brain tissue. This can happen when a bullet or knife makes a hole in the skull and enters the brain.
The Brain
The brain is a three pound, gelatinous organ housed in the skull. Each side of your brain has four lobes and they’re sensitive to trauma. TBI can be localized to a certain part of the brain or the trauma can involve more than one area of the brain incapacitating their function. What follows is a brief account of the normal function of the cerebral lobes.
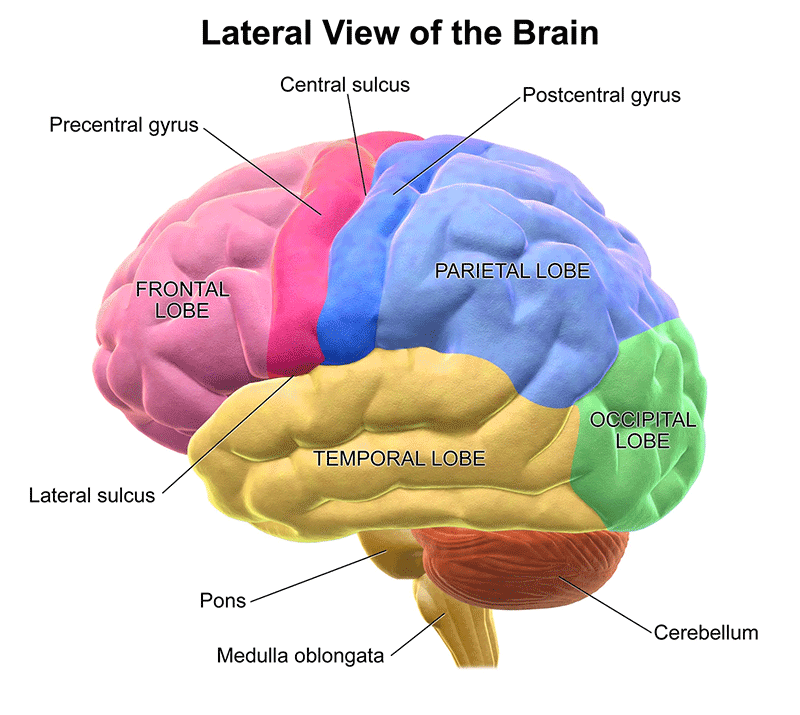
- The frontal lobe is the largest of the four lobes and is located, as the name indicates, at the front of the brain. It’s involved with memory and thinking, making decisions (judgment, and reasoning) and social interactions. The frontal lobe is also involved with voluntary movements, emotional expression, motivation and is related to speech.
- The temporal lobe plays an important role in hearing as well as in speech and language production. It processes memories and makes memory associations.
- The occipital lobe is the smallest of the four lobes and is located in the back of the brain. Its main function deals with vision and processing visual stimuli.
- The parietal lobe processes information about movement, taste, temperature, and touch. It’s responsible for integrating sensory input with the visual system.
The location and severity of the brain injury vary and it can interfere with your ability to think, remember, speak, move about and act reasonably. It may affect your hearing or vision, cause dizziness, persistent headaches and provoke seizures.
After such trauma, your impulse control switch in the frontal lobe may be short-circuited and your behavior, emotions, and reactions can become outlandish.
The neurologist Steven Lawreys used the phrase “Shake It and You Brake It” to emphasize the damage closed head trauma inflicts on the brain.
At times, the news media reports an ignorant parent or some adult picking up a baby and vigorously shaking him or her for misbehaving or crying too much. All too often, such trauma has caused irreparable brain damage Shaking a child can result in damage similar to a closed brain injury, in this instance, called “shaken baby” syndrome.
Although head trauma can happen to anyone at any age, those most at risk to experience TBI are young people between 10 and 24 years of age and people over the age of 75.
The causes of TBI vary and include traffic accidents, being assaulted, blast injuries, falls or accidents at home or at work. The symptoms depend on the location and the extent of damage to the brain. The symptoms of TBI can be mild, moderate or severe. Some symptoms or signs may appear right after the head trauma, while other symptoms might appear days or weeks later (see Mild TBI symptoms below).
Diffuse Axonal Injury (DAI)
DAI is a common type of traumatic brain injury that often occurs after an auto accident, sports injury or falls. The brain nerve fibers (axons) are damaged as it twists and turns after blunt injury to the brain. This type of injury usually results in a person being unconscious or in a coma affecting different parts of the brain.
‘Mild’ Traumatic Brain Injury
Not all head bumps or jolts to the head result in lasting damage to the brain. But if you hit your head on a door or bang your head on the ground, you might complain of symptoms such as headache, nausea, vomiting confusion and being disoriented.
The blow to the head might cause you to forget what happened immediately before or after the accident (amnesia). In addition, dizziness, imbalance and a brief period of unconsciousness lasting several minutes may occur. Also, people have been troubled by mood disturbances, irritability and difficultly concentrating. Approximately 75-80% of all head injuries are attributed to mild TBI.
Moderate-Severe Traumatic Brain Injury
People with moderate or severe traumatic brain injury experience many of the symptoms of mild TBI. ‘Moderate’ TBI has been described as a “loss of consciousness between 15 minutes to six hours or a period of post-traumatic amnesia of up to 24 hours.
‘Severe’ TBI is an extended period of unconsciousness or amnesia after brain injury. It’s the condition where the patient has been in an unconscious state for six hours or more, or a post-traumatic amnesia of 24 hours or more.” In other words, severe TBI can result in a long-lasting coma or a persistent vegetative state.
Everyone is at risk for traumatic brain injury. Whether you’re a baby or over the age of 75, a professional athlete or a veteran, head trauma can and has caused serious injuries with long term consequences.
If you’ve received a serious blow to the head, seek immediate medical assistance; especially if you were unconscious, disoriented, confused or forgot events before or after the head injury. “Shake it and You Break It.” is a reminder that a seemingly minor head trauma can have damaging long term effects on your thoughts, emotions, behavior, and your ability to concentrate and communicate.
References
- Centers for Disease Control and Prevention (2019); Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014.
- Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury—Related Emergency Department Visits, Hospitalizations, and Deaths — United States, 2007 and 2013. MMWR Surveill Summ 2017
- National Institute of Neurological Disorders and Stroke; Traumatic Brain Injury Information Page; March 3, 2019
- Centers for Disease Control & Prevention; Brain Injury Basics; March 5, 2019
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.

