Joseph R. Anticaglia, MD
Medical Advisory Board
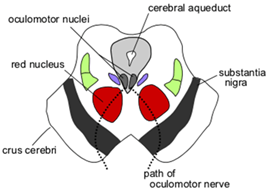
Parkinson disease (PD) is a disorder within the brain that develops slowly over the years. This progressive, degenerative neurological disease happens when certain nerve cells in part of the brain called the substantia nigra (black substance) die earlier than normal and do not produce sufficient amounts of dopamine.
Dopamine is the chemical messenger needed to relay crucial information between nerve cells in the brain (neurotransmitter). We need sufficient amounts of this chemical substance to control our movements and maintain our posture and balance.
When there is less and less dopamine available, more brain cells die or malfunction which can cause an increase in abnormal movements of the body and a paucity of voluntary or involuntary movements. It is often referred to as a movement disorder (motor) but there are other debilitating, non-movement (non-motor) PD symptoms associated with a depletion of dopamine.
Who gets Parkinson’s disease?
PD affects young and old, rich, and poor, men and women without discrimination to ethnicity. It’s estimated that 60,000 Americans each year are diagnosed with this disease. About a million Americans have PD, men more than women. The onset of PD typically occurs between 45 and 65 years of age, more frequently after the age of sixty. Asians and African Americans are less likely to develop Parkinson’s
You might recognize some individuals diagnosed with Parkinson’s, for instance: Michael J. Fox (diagnosed at age 29), Alan Alda. Reverend Billy Graham, Janet Reno, Pope John Paul 2nd, Johnny Cash, Muhammad Ali, Linda Ronstadt, President George H. W. Bush, Robin Williams and, of course, many more.
Risk Factors for Parkinson Disease include:
- Age People usually develop PD after the age of sixty. As we age, there is a loss of dopamine producing cells in the substantia nigra affecting our movement and non-movement abilities. Young adults rarely experience Parkinson’s disease.
- Genetics Family history, after age, seems to be a strong predictor to the development of PD.
- Gender Men are more prone to develop PD than women
- Exposure to toxins may increase your risk to develop Parkinson’s disease, for instance, pesticides/herbicides, MPTP — a synthetic neurotoxin, and possibly agent orange
- Medications’ side effects, for instance, drugs used for seizures, nausea and vomiting, antidepressants, and others
- Head trauma
A sixty-six page scientific treatise written to pay tribute to London physician James Parkinson was published in 1817 titled, “An Essay on the Shaking Palsy.” He was the first person to document this disease. The paper described a nervous system disorder, according to an article in Brain magazine, “characterized by a trembling of the limbs at rest, lessened muscular power and a stooped posture associated with a propulsive,” involuntary quickening of a person’s manner of walking.
Symptoms
Parkinson’s disease weighs down each person and each family member differently. No one gets all the symptoms of PD, and they vary according to the stage of the disease.
Two types of Parkinson’s symptoms:
- Motor symptoms (affect the movement of patients)
- Non-motor Symptoms
Key Motor Symptoms
- Tremor — shakiness or involuntary shaking which is more pronounced at rest
- Bradykinesia — slowness or absence of movement.
- Rigidity — muscle stiffness or inflexibility of arms, legs and/or trunk.
- Postural Instability — poor balance
- Freezing or Walking/gait problems
Tremor (shakiness) is the involuntary quivering or shaking movement of the body or limbs. It’s present in about 70% of PD patients and it most often involves the hand, ankle, foot, leg, or chin. It is more noticeable at rest (resting tremor) and is exacerbated by emotional stress, fatigue and is less severe or disappears during voluntary, intentional movement such as shaking hands.
In general, the tremor starts in one limb, the upper limb or on one side of the body. Characteristically, it involves the hand which takes the appearance of a pill rolling movement between the thumb and forefinger. In the lower limb, tremor is most noticeable at the ankle — foot. It can spread to the other side after months or years of having the disease. The tremor usually disappears during sleep.
Bradykinesia (slowness) refers to profound slowness of voluntary movement or a reduction of autonomic movement which may include slowness of chewing, swallowing, constipation or a reduction or absence of swinging of the arms. Incoordination may be present as seen when patients have difficulty brushing their teeth. Puzzlingly, sufficient voluntary activity can be regained briefly in an emergency, for instance, to avoid an oncoming car.
Another movement symptom, rigidity is experienced by PD patients as (stiffness or tightness) of muscles involving the arms, legs or body which is worse than that of normal aging. There is restricted turning movement of the spine and people have complained of cramps and muscle spasms.
Postural instability is being off balance with a tendency to fall which occurs later in the disease process. People with PD can display walking problems such as a festinating gait — walking with quick, small shuffling steps, as if in a hurry.
Freezing is the sudden, temporary inability of PD patients to move or ambulate. It can happen anytime and anywhere; for instance, when walking, you suddenly stop and can’t take another step (freezing gait), you cannot rise from a chair, or you have trouble turning. In short, you have the feeling of being “stuck in place” when attempting to wail or move
The diagnosis of Parkinson’s disease is a clinical one. In order to make the diagnosis of PD, bradykinesia plus either tremor or rigidity must be included in the other key symptoms. A strong indicator of primary PD is the unilateral onset of a pill-rolling resting tremor. Another strong clinical clue indicating primary PD is the powerful, positive response to the drug levodopa in calming the motor symptoms of Parkinson disease. However, non-motor symptoms can, at times, be more troublesome to patients than motor symptoms.
Parkinson Disease’s ‘Other’ Motor Signs and Symptoms include:
- Pill rolling movement between the thumb and forefinger
- Decreased automatic reflexes, such as reduced blinking
- Dysknesia — involuntary, writhing-squirming movements of the face, arms, legs, or trunk, e. g., Michael J. Fox
-
Stooped posture

Illustration of PD by William Richard Gowers - Facial masking — Loss of facial expression due to rigidity of facial muscles, also called hypomimia, e. g., Muhammad Ali
- Festinating gait — Walking with a series of quick, small, shuffling steps, as if in a hurry
- Low voice volume, muffled or unclear speech, called dysarthria
- Dystonia — cramping or tightening of a muscle(s).
- Slight foot drag on the affected side
-
Microgrphia — Small, cramped handwriting
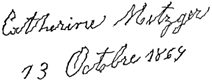
Jean-Martin Charcot 1879 Handwriting of a person affected by PD - Retropulsion — Tendency to fall backwards
- Sialorrhea (drooling) — slowness of muscle movement during chewing or swallowing
- Difficulty getting up from a chair or turning over in bed
If conspicuous movement behaviors are not controlled by medication, surgical treatment may be considered after consultation with a movement disorder Neurologist.
Deep Brain Stimulation (DBS) involves implanting thin wires called electrodes into one or both sides of the brain that control movement. These electrodes are connected to a small battery device in the chest that sends electrical signals to the brain to resolve the problem. Some refer to it as a pacemaker for the brain.
Parkinson’s disease impacts people from all walks of life and backgrounds. The exact cause of PD is unknown although genetics, exposure to toxins, head trauma and certain antipsychotic medications have been associated with PD. Presently there is no cure for this disease; however, there are medications which reduce the symptoms of this disease.
If you suspect you have Parkinson disease, it’s advisable to be examined by a neurologist; especially one with additional training is movement disorders. It’s important to realize you will not die from Parkinson disease and nobody develops all the symptoms of PD. Your unique experience, symptoms and disease progression will be similar but quite different from people you meet with PD.
At present, active research is ongoing in the diagnosis, treatment and potential cure for PD. The Parkinson ‘Foundation and he Michael J. Fox Foundation for Parkinson’s Research are two of several sources to get information about clinical trials.
Glossary
Primary Parkinson’s disease and Paralysis agitans are other names for Parkinson Disease. It’s the prototype for this condition
Parkinsonism refers to other conditions that result in tremor and rigidity. These Secondary conditions, such as, toxic tremor, familiar tremor or spasticity should be distinguished by a neurologist from Primary Parkinson’s disease.
References
- Andrew Lees; An Essay on the Shaking Palsy; Brain, February 24, 2017
- Stephen K. Van Den Eeden et al; Incidence of Parkinson’s Disease: Variation by Age, Gender, and Race/Ethnicity; Am J of Epidemiology, June1, 2013
- Christopher G. Goetz; The History of Parkinson’s Disease: Early Clinical Descriptions and Neurological Therapies; Cold Spring Harb Perspect Med. Sep 1, 2011
- National Institute of Neurological Disorders and Stroke; Parkinson’s Disease Information Page; 2019
- National Institute of Neurological Disorders and Stroke; Parkinson’s Disease: Hope Through Research; 2019
- Parkinson Foundation: What is Parkinson’s Disease?
- Michael J. Fox Foundation for Parkinson’s Research
- Min Wen et al; Serum uric acid I patients with Parkinson Disease; Plos ONE, March 20, 2017
- Lazaros C. Triarhou; Dopamine and Parkinson’s Disease; Madame Curie Bioscience Database [Internet]
- Gale Kittle, RN, MPH; What You and Your Family Should Know About Parkinson’s Disease; Parkinson’s Foundation
- Alberts JL, Linder SM, Penko AL, Lowe MJ, Phillips M: It is not about the bike, it is about the pedaling forced exercise and Parkinson’s disease. Exerc Sport Sci Rev 2011.
- Anne S. Berry et al; Aging Affect Dopaminergic Mechanisms of Cognitive Flexibility; Journal of Neuroscience, Dec 14, 2016
Addendum
Another post will discuss the non-motor symptoms.
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.

