Joseph R. Anticaglia MD
Medical Advisory Board
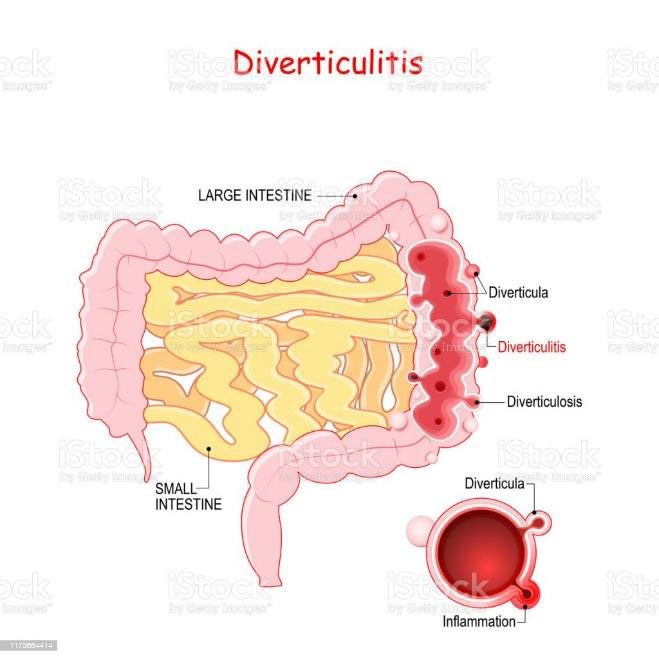
Diverticular disease is a disease of the large intestine characterized by tiny outpouchings in the wall of the colon called diverticula, which can become inflamed (red, swollen) and infected. This colonic disease affects approximately half of the population over the age of 60 in advanced western countries. It was thought to be a disease of the elderly, but recent reports indicate an increased prevalence in persons younger than 60 years of age. The disease is divided into diverticulosis and diverticulitis.
A) Diverticulosis is the existence of those outpouchings or pouches that bulge through the colonic wall. The outpouchings vary in size and number. Most of the time, they are discovered accidentally on X-ray examination or during a colonoscopy done to screen for cancer. More than 90% of the people with diverticulosis have no pain or symptoms. The diverticula are not infected. Individuals might have symptoms of bloating, constipation, abdominal discomfort or a change in bowel habits.
B) Diverticulitis occurs when the outpouchings of the colon become inflamed and infected. With this condition, there are the potential complications of bleeding, abscess formation, fistula formation and perforation of the wall of the colon. The symptoms are thought to be caused by bacteria becoming trapped inside the bulging wall of the colon.
Symptoms of diverticulitis range from mild abdominal aching and tenderness to acute cramping abdominal pain. The most common symptom is lower left sided belly pain. If infection is present, individuals may experience fever, nausea, vomiting diarrhea or constipation as well as blood or mucous in the stool.
The Cause of diverticular disease’s outpouchings is uncertain. However, you are at an increased risk to get this disease if you’re an obese male over the age of sixty who smokes, doesn’t exercise, takes steroids or uses nonsteroidal anti-inflammatory drugs (Advil, Aleve, or Motrin). Chronic constipation causes increased pressure in the colon and is thought to predispose to diverticula.
The diagnosis of diverticular disease is made by using your medical history physical examination and certain tests. Your history of acute abdominal pain and fever, tenderness in the region of the left lower abdomen and a possible mass in that area make your doctor want to order certain tests that might include:
- CT scan (computed tomography) of the abdomen checks for diverticulitis, plus other problems
- A barium enema, [a lower gastrointestinal (G. I.) series], evaluates the presence of diverticula, growths, tumors or narrowing of the intestine.
- Stool samples look for blood, bacteria or parasites that might be the cause of fever or bleeding.
- Blood tests check for a certain elevated white blood count (leukocytosis) that indicates an infection.
- A Colonoscopy allows your doctor to examine your large intestine.
Complications of Diverticulitis
Acute or chronic inflammation of the colon can cause narrowing of the intestine with partial or complete obstruction. Untreated abscess or chronic inflammation can lead to bleeding, bowel obstructions or perforations which might contaminate nearby organs. In addition, chronic infection or an untreated abscess can lead to fistulas, openings that connects the infected large intestine with another body part such as the vagina, bladder or abdominal wall.

Treatment of Diverticulitis
Home Treatment
If you are healthy individual with mild symptoms of diverticulitis, you can often be successfully treated at home with a liquid diet and pain medication. However, you should seek medical attention if you cannot tolerate the liquid diet, if you spike a temperature above 101F or you experience worsening left sided abdominal pain.
Hospital Treatment
If you are in poor health, if your symptoms don’t improve in 2 or 3 days with home treatment or if you have severe disease, you may need to be hospitalized for treatment. You’ll be NPO (nothing by mouth) initially. Fluids and antibiotics will be administered intravenously.
Surgery
Surgical intervention is considered as a last resort for diverticulitis. An abscess of the colon may have to be surgically drained to manage the patient’s condition. Emergency surgery may be warranted if the person develops peritonitis, a generalized infection of the abdomen. Other indications for surgery include recurrent episodes of diverticulitis not responsive to medical treatment and complications such as fistula, perforation and bowel obstruction.
Diverticular disease occurs when individuals have symptoms due to diverticulosis (the outpouchings of the wall of the colon) or diverticulitis (when the pouches become inflamed or infected). Although the cause of diverticular disease is unknown, a high fiber diet helps to prevent constipation and the formation of diverticula that may progress to diverticulitis. Most cases are treated as outpatients with diet and medications, but severe cases require hospitalization.
References
- N. Stollman, J B Raskin; Diverticular Disease of the Colon; The Lancet, 2004
- Rezapour, Mona et al; Diverticular Disease: An Update on Pathogenesis and Management; Gut and Liver; March 2018
- Sophia M. Swanson and Lisa L. Strate; In the Clinic: Acute Colonic Diverticulitis Ann Intern Med. May 1, 2018
- Weizman, Adam and Nguyen Geoffrey; Diverticula Disease: Epidemiology and Management; Can J Gastroenterology, July 2011
- Peery, AF et al; Distribution and characteristics of colonic diverticula in the United States screening population; Clin Gastroenterol Hepatol; July 2016
Glossary
Fistula — an abnormal connection between two areas that are not normally connected (e. g..) colon and bladder).
Peritonitis — infection involving the space around the abdominal cavity.
Abscess — a localized collection of pus
This article is intended solely as a learning experience. Please consult your physician for diagnostic and treatment options.

